Tinea Capitis: Causes, Symptoms & Treatment | Scalp Ringworm Guide
Introduction to Tinea Capitis
Tinea Capitis, commonly known as scalp ringworm, is a fungal infection that affects the skin on your scalp. This condition is caused by dermatophytes, a group of fungi that thrive on keratin, a protein found in hair, skin, and nails. The infection can lead to patches of hair loss, itching, redness, and scaling on the scalp. Tinea Capitis is highly contagious, meaning it can spread from person to person through direct contact or by sharing contaminated objects like combs, hats, or towels.
It’s important to understand that Tinea Capitis is not a sign of poor hygiene; anyone can get infected, and it is often more common in children, especially in crowded environments like schools or daycare centers.
Importance of Awareness
Being aware of Tinea Capitis is crucial because, when left untreated, this fungal infection can lead to long-term hair loss and scarring. It’s essential for individuals to recognize the symptoms early and seek treatment. If the infection spreads or is left unmanaged, it can result in permanent damage to the hair follicles, causing lasting bald patches. Additionally, untreated Tinea Capitis can affect your overall well-being due to persistent itching and discomfort. Early intervention helps prevent complications, minimizes the risk of spreading the infection to others, and ensures quicker recovery.
Who is at Risk?
While anyone can contract Tinea Capitis, certain groups are more prone to the infection. The primary risk factors include:
-
Children: Children aged 3-14 are at a higher risk, especially those in close contact with others at school, daycare, or sports.
-
Individuals with weakened immune systems: People with conditions such as HIV/AIDS or those on immunosuppressive medications are more susceptible.
-
Close contact with infected individuals: Tinea Capitis spreads easily in communal areas, so frequent contact with someone who has the infection increases the risk of transmission.
-
Living in crowded conditions: Sharing personal items like hairbrushes, towels, and hats, or living in environments like boarding schools or shelters increases the likelihood of coming into contact with the infection.
Additionally, pets—especially cats and dogs—can sometimes harbor the fungi that cause Tinea Capitis, leading to zoonotic transmission.
Common Misconceptions
There are several misconceptions about Tinea Capitis that can delay proper treatment:
-
“Only dirty people get Tinea Capitis”: Many believe that poor hygiene is the cause of this fungal infection, but the truth is that anyone can get Tinea Capitis, regardless of cleanliness. The infection is caused by fungi, not a lack of hygiene.
-
“Tinea Capitis affects only children”: While it’s more common in children, adults are also susceptible to this condition. Individuals in close contact with children or those living in crowded spaces should be aware of the risk factors.
-
“Tinea Capitis causes permanent baldness”: Another misconception is that Tinea Capitis leads to permanent hair loss. If caught and treated early, the hair usually grows back, and permanent damage can be avoided. However, delaying treatment increases the likelihood of scarring and permanent hair loss.
-
“Tinea Capitis is just dandruff”: Tinea Capitis is often confused with dandruff, but the two are very different. While dandruff is a mild scalp condition related to dry skin or seborrheic dermatitis, Tinea Capitis is a fungal infection requiring antifungal treatment.
By understanding the realities of Tinea Capitis, individuals can better protect themselves and others from this common, but preventable, scalp infection.
Causes and Pathogenesis
Tinea Capitis is caused by a group of fungi known as dermatophytes, which thrive on keratin, the protein found in hair, skin, and nails. These fungi infect the scalp, leading to symptoms such as hair loss, itching, redness, and scaling. The condition is a form of fungal scalp infection, which is commonly referred to as scalp ringworm. It primarily affects the hair follicles and the surrounding skin, causing inflammation and sometimes hair loss in affected areas.
Tinea Capitis is often more severe in children, but it can also affect adults, especially those with compromised immune systems. The fungi invade the hair follicles and feed on the keratin, causing the scalp's outer layer to become inflamed and itchy. Without proper treatment, the infection can lead to scarring and permanent hair loss.
Types of Fungi Involved (Dermatophytes: Microsporum, Trichophyton)
The fungi that cause Tinea Capitis are dermatophytes, specifically species from the Microsporum and Trichophyton genera. These fungi have a natural affinity for keratin and are responsible for a variety of fungal infections that affect the skin, nails, and hair. The two main types of dermatophytes involved in Tinea Capitis are:
-
Microsporum: This genus includes Microsporum canis, which is the most common cause of Tinea Capitis, especially in cases where the infection is contracted from animals. It is usually associated with animal-to-human transmission, often from pet cats or dogs.
-
Trichophyton: Another genus of dermatophytes, including species like Trichophyton tonsurans, which is responsible for the majority of human-to-human transmissions. Trichophyton is often the cause of Tinea Capitis in children and is more commonly spread in schools and daycare centers.
Both types of fungi thrive in warm, moist environments, making the scalp a prime target. They can survive in the environment for an extended period, which means they can remain on contaminated surfaces like combs, towels, and hats, contributing to the infection's spread.
How the Infection Develops (Pathogenesis)
The pathogenesis of Tinea Capitis begins when the dermatophytes come into contact with the scalp and begin to colonize the hair follicles. The fungi invade the outer layers of the skin, particularly the stratum corneum, and feed on the keratin present in the hair and skin cells.
As the infection progresses, the fungi produce enzymes that break down the keratin, leading to inflammation and scalp irritation. The scalp may become red, scaly, and itchy, with hair loss in the infected areas. In severe cases, the infection can lead to pustules or abscesses on the scalp, and if untreated, the hair follicles can become permanently damaged, leading to scarring and permanent bald patches.
In some cases, the infection can spread to nearby areas of the skin, especially if the affected person scratches the scalp, potentially allowing the infection to spread to their hands, nails, or body.
Transmission: How Does It Spread?
Tinea Capitis is highly contagious, and its transmission can occur through various methods:
-
Direct Contact: The most common way Tinea Capitis spreads is through direct skin-to-skin contact with an infected person. Children are particularly vulnerable in school or daycare settings, where close contact with classmates is common.
-
Indirect Contact: The fungi can also be spread through contaminated objects, such as combs, brushes, hats, towels, and bed linens. Sharing these items with an infected individual can lead to the spread of the infection.
-
Animal-to-Human Transmission: Tinea Capitis can also spread from pets to humans, particularly from cats or dogs that carry the fungi. These animals may not show symptoms but can still harbor the dermatophytes, transmitting them to humans when they come into contact with their fur.
-
Environmental Exposure: Fungal spores from Tinea Capitis can live in the environment for months, allowing indirect transmission via contaminated surfaces. Public spaces like locker rooms or swimming pools can also act as breeding grounds for the fungi.
Risk Factors (Age, Immunity, Environment, Animal Contact, Crowded Living)
Several factors increase the likelihood of contracting Tinea Capitis, including:
-
Age: Children, especially those between 3 and 14 years old, are at a higher risk due to their increased interaction with other children in places like schools, daycare centers, and sports activities. However, adults can also develop the infection, particularly if they are frequently in contact with infected children or animals.
-
Immunity: Individuals with weakened immune systems, such as those with HIV/AIDS, cancer, or those undergoing immunosuppressive treatments (like chemotherapy or steroids), are more susceptible to fungal infections, including Tinea Capitis.
-
Environmental Exposure: Living in crowded conditions, such as in shelters, dormitories, or boarding schools, increases the risk of exposure to Tinea Capitis. Public facilities like swimming pools or gyms, where people share towels and equipment, can also increase the chances of infection.
-
Animal Contact: Having close contact with infected animals, particularly cats and dogs, significantly increases the risk of contracting Tinea Capitis. This is especially true if the animal shows signs of skin infection or if the fungi are transmitted via the animal's fur.
-
Poor Hygiene: While poor hygiene is not a direct cause of Tinea Capitis, individuals with unwashed hair or skin may be more prone to fungal infections due to the increased opportunity for the fungi to colonize. Moreover, individuals who are unaware of the infection's contagious nature may spread the fungi without realizing it.
By understanding these risk factors, individuals can take proactive steps to reduce their chances of contracting Tinea Capitis. Recognizing the signs and symptoms early can help in seeking treatment and preventing the infection from spreading to others.
Epidemiology
Global Prevalence and Distribution
Tinea Capitis, or scalp ringworm, is a common fungal infection that affects individuals worldwide, with higher prevalence rates in developing countries. Globally, it is estimated that 10-20% of children under the age of 12 are affected by this infection, although adults can also contract Tinea Capitis, particularly in environments where there is close contact with infected individuals or animals. The prevalence of Tinea Capitis varies depending on geographical location, environmental conditions, and socio-economic factors.
In tropical and subtropical regions, the infection rate tends to be higher due to the warm and humid climate, which provides an ideal environment for fungal growth. In these regions, Tinea Capitis can affect both children and adults, with children being the most vulnerable group. This is particularly true in communities with poor sanitation or where overcrowded living conditions increase the risk of transmission.
In developed countries, the rates of Tinea Capitis have declined due to better hygiene practices, increased awareness, and more advanced medical treatments. However, outbreaks still occur, especially in school-aged children or those who live in close-knit communities. Moreover, the rise of immune-compromised populations has contributed to an increase in adult cases in some parts of the world.
Age and Gender Patterns
Tinea Capitis primarily affects children, particularly those between the ages of 3 and 14. This age group is at an increased risk due to their regular interaction with other children in environments such as schools, daycare centers, and sports teams, where the infection can spread quickly. Children are more likely to share personal items such as combs, hats, and towels, which can carry fungal spores.
While Tinea Capitis is more common in children, adults are also susceptible to the infection, particularly if they have frequent contact with infected individuals or animals. In adults, the infection is more likely to occur in those with weakened immune systems or those living in crowded conditions where there is increased exposure to the fungi.
Regarding gender, males tend to have a slightly higher prevalence of Tinea Capitis during early childhood. However, as children grow older, the difference in prevalence between genders diminishes. In adults, Tinea Capitis is more common in females, particularly among those who are immune-compromised or have chronic underlying health conditions.
High-Risk Populations (Children, Adults, Immunocompromised)
Certain populations are more at risk for developing Tinea Capitis due to a combination of environmental, genetic, and health-related factors. These high-risk groups include:
-
Children: Children are by far the most vulnerable group for Tinea Capitis. Their underdeveloped immune systems and frequent close contact with peers in places like schools and daycare centers make them highly susceptible. Children under the age of 12 have a higher risk of developing Tinea Capitis because of their increased exposure to infected individuals and animals.
-
Immunocompromised Individuals: People with weakened immune systems are at an increased risk of developing various fungal infections, including Tinea Capitis. This includes individuals with HIV/AIDS, those undergoing chemotherapy, and people on immunosuppressive treatments like steroids or organ transplant medications. In these individuals, the body's ability to fight off fungal infections is compromised, making them more susceptible to severe and persistent infections.
-
Adults in High-Risk Environments: Adults who live in overcrowded or communal environments—such as homeless shelters, prisons, or refugee camps—are also at a higher risk. The constant proximity to others increases the likelihood of direct contact with an infected individual, as well as exposure to contaminated surfaces, towels, or personal items.
-
Animal Handlers: People who frequently handle animals, particularly cats and dogs, are at an increased risk of contracting Tinea Capitis. In some cases, animals—especially those with no visible symptoms—can carry the dermatophytes that cause the infection, transmitting them to humans through direct contact with their fur or skin.
Geographic and Socioeconomic Factors
Geographic location plays a significant role in the prevalence and spread of Tinea Capitis. In areas with warmer climates, particularly in tropical and subtropical regions, the infection rates are higher due to the environmental conditions that favor the growth of dermatophytes. These areas often have high humidity, which provides an ideal environment for fungal spores to thrive. Regions with poor sanitation and overcrowded living conditions further increase the risk, as individuals are more likely to come into contact with contaminated surfaces or other infected individuals.
Socioeconomic factors also contribute to the spread of Tinea Capitis. In areas where poverty, limited access to healthcare, and poor hygiene practices are prevalent, the infection is more likely to spread. Overcrowded living conditions, particularly in urban slums, can further facilitate the transmission of Tinea Capitis. Poor access to antifungal treatments and awareness about proper hygiene and infection prevention can also contribute to the high incidence of the disease in such populations.
On the other hand, in developed countries, where hygiene practices are better and healthcare systems are more accessible, the prevalence of Tinea Capitis is lower. However, the condition can still occur in certain high-risk groups, particularly in children and individuals who are immunocompromised. Additionally, immigration from regions with high Tinea Capitis prevalence can introduce the infection into new areas, especially if individuals are unaware of how the condition spreads or how to prevent it.
Types and Clinical Variants of Tinea Capitis
Tinea Capitis, also known as scalp ringworm, has various clinical presentations and can be classified into different types based on the severity of the infection and the appearance of the affected scalp. These types include inflammatory and non-inflammatory forms, each of which has its own set of characteristics and treatment challenges. Here, we will discuss the most common types and clinical variants of Tinea Capitis.
Inflammatory vs. Non-Inflammatory Types
Tinea Capitis can be divided into two main categories based on the presence of inflammation:
-
Inflammatory Tinea Capitis: This type is characterized by significant inflammation, redness, swelling, and sometimes the formation of abscesses or pustules on the scalp. The infection can cause severe itching, pain, and even drainage of pus in more advanced cases. Inflammatory Tinea Capitis is typically associated with more severe fungal infections, often requiring more aggressive treatment to resolve.
-
Non-Inflammatory Tinea Capitis: In contrast, non-inflammatory Tinea Capitis involves a less severe infection, with fewer visible symptoms. The scalp may show signs of hair loss and mild scaling, but there is typically no significant redness or swelling. Non-inflammatory Tinea Capitis tends to be less painful and may resolve with standard antifungal treatments.
Black Dot Tinea Capitis
Black Dot Tinea Capitis is a common form of non-inflammatory Tinea Capitis, typically seen in children. It is named for the distinctive appearance of black dots on the scalp, which are actually broken hair shafts that remain lodged in the follicles. This condition is primarily caused by Trichophyton tonsurans, a dermatophyte fungus that invades the hair shafts, causing them to break off at the surface of the scalp. The broken hairs give the scalp a dotted appearance, which can be mistaken for dandruff or other hair loss conditions.
This type of Tinea Capitis often presents with mild symptoms, including slight scaling, but can cause progressive hair loss over time if left untreated. While it typically doesn’t cause pain or significant inflammation, it can be frustrating for both children and adults, especially if the condition is persistent.
Gray Patch Tinea Capitis
Gray Patch Tinea Capitis is another non-inflammatory form, commonly caused by Microsporum species of dermatophytes, especially Microsporum canis, which can be transmitted from pets. It is characterized by the development of round, scaly patches on the scalp with a grayish appearance. These patches often have a balding center and a scaly ring around the edges, making it resemble a ringworm infection.
Gray Patch Tinea Capitis is typically less painful than inflammatory types, but it can still cause noticeable hair loss, which may be distressing for the person affected. The infection tends to progress more slowly than other forms of Tinea Capitis and can be diagnosed through microscopic examination or fungal cultures.
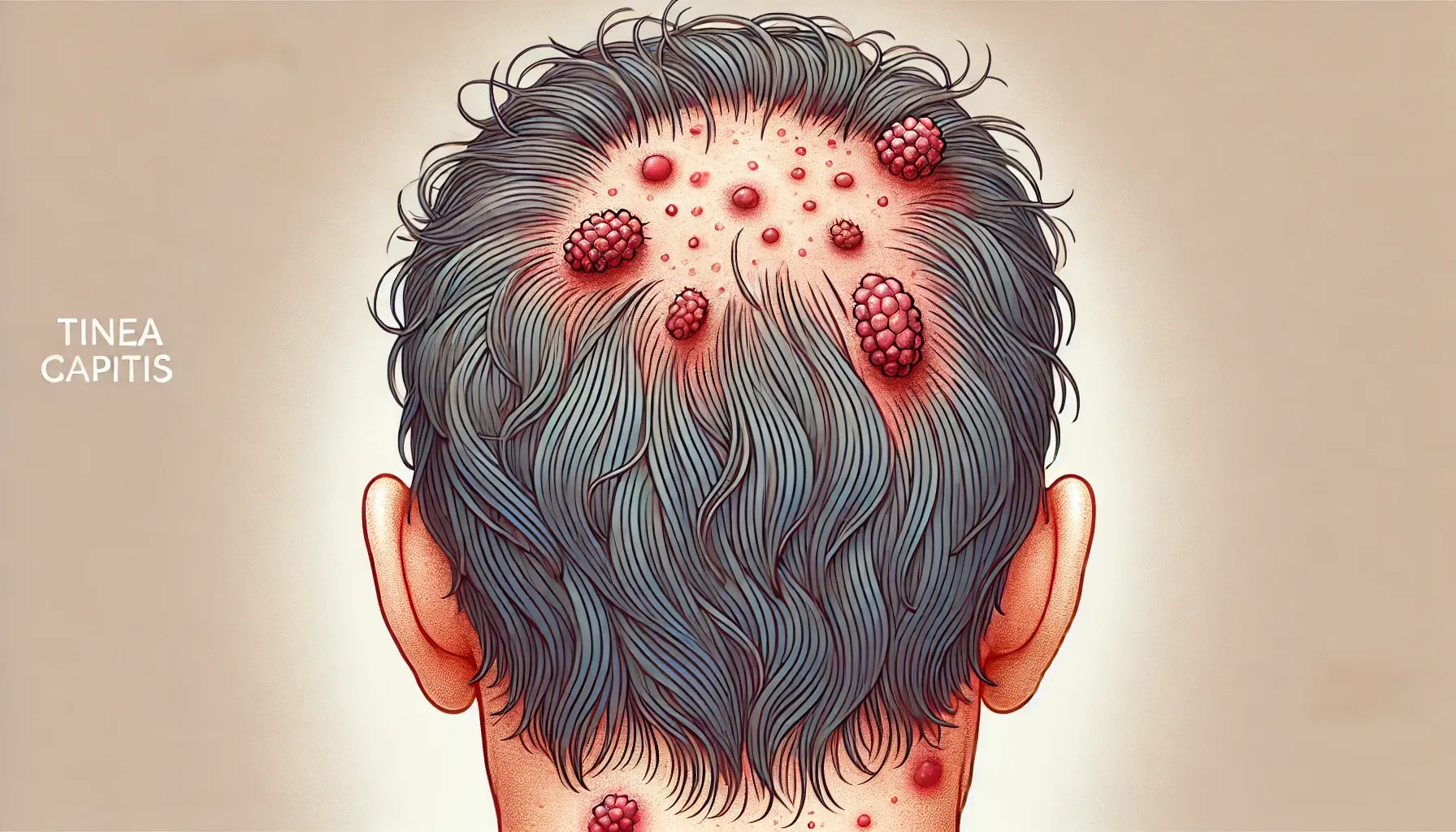
Kerion (Severe Inflammatory Reaction)
Kerion represents the most severe form of inflammatory Tinea Capitis. It occurs when the fungal infection triggers a strong immune response in the affected area. This leads to the formation of large, painful, pus-filled abscesses on the scalp, often accompanied by intense redness, swelling, and hair loss. Kerion is typically caused by Trichophyton mentagrophytes or other dermatophytes and is more common in children, although adults can also develop it, particularly if they have compromised immune systems.
Kerion is considered a medical emergency because it can lead to permanent hair loss and scarring if not treated promptly. The infection can also be complicated by secondary bacterial infections, making it essential to seek aggressive antifungal treatment, often combined with antibiotics, to manage the inflammation and prevent long-term damage.
Favus (Chronic Type)
Favus is a rare but chronic form of Tinea Capitis that can persist for months or even years if left untreated. It is caused by a type of Trichophyton fungus and is most commonly seen in areas with poor sanitation or overcrowded living conditions. Favus is characterized by the formation of yellowish, crusty patches (scutula) on the scalp, which emit a foul odor. Over time, these patches can lead to permanent scarring and hair loss.
Favus is often accompanied by a generalized sense of discomfort, including itching and tenderness. If the infection is not treated early, it can lead to widespread hair loss and even permanent damage to the hair follicles. This chronic form is more common in children but can affect adults in high-risk environments.
Differences in Adults vs. Children
The presentation and severity of Tinea Capitis can differ significantly between adults and children:
-
In Children: Tinea Capitis is more common, especially in children aged 3 to 14. It is often transmitted through direct contact with other infected children or pets, especially in school or daycare environments. In children, the infection tends to be less painful but can cause significant hair loss. Non-inflammatory types like Black Dot Tinea Capitis and Gray Patch Tinea Capitis are more common in children, with the latter often being associated with animal contact.
-
In Adults: Tinea Capitis is less common in adults but can occur in those who are immune-compromised, such as those with HIV, diabetes, or those undergoing chemotherapy. Adults tend to experience more severe forms of the infection, such as Kerion, which may cause more pain and scarring. In adults, Tinea Capitis may also take longer to heal due to the weakened immune system or delayed treatment.
Key Differences in Clinical Features:
-
In Children: The infection tends to be milder, with more cases of non-inflammatory forms. It may cause temporary hair loss, but complete regrowth is possible with treatment.
-
In Adults: The infection tends to be more severe, with a higher risk of complications like Kerion or scarring. Adults may also face challenges in seeking early treatment, leading to more persistent infections.
Signs and Symptoms
Tinea Capitis, commonly known as scalp ringworm, progresses through various stages. The symptoms can range from mild to severe, and recognizing them early is key to preventing further complications. This fungal infection typically affects the scalp, leading to a range of visible and sometimes painful symptoms. Let’s break down the signs and symptoms of Tinea Capitis.
Early Symptoms (Itching, Flaking, Redness)
The early stages of Tinea Capitis are often subtle, with the most common symptoms being itching and scaling of the scalp. These symptoms can be mistaken for dandruff or dry skin, which is why it’s important to stay alert to changes in your scalp’s condition.
-
Itching: One of the first noticeable signs is persistent itching on the scalp, which can range from mild irritation to a more intense, constant sensation. The itching may get worse as the infection spreads.
-
Flaking: As the infection begins to take hold, you may notice scaling or flaking of the skin on your scalp, similar to dandruff. The scales may be white or slightly yellowish and can be found along with the itchy patches.
-
Redness: The scalp may become red or inflamed in the early stages as the body’s immune system reacts to the fungal infection. This redness is typically mild at first but can worsen if the infection is left untreated.
Progression of the Disease
As the infection progresses, the symptoms of Tinea Capitis become more pronounced. Early signs of flaking and itching develop into more noticeable changes in the scalp’s appearance and the health of the hair.
-
Scaling and Crusting: The scales on the scalp may become thicker and more pronounced, and in some cases, they may form crusts. These crusts are often yellowish in color and can be seen around the edges of the affected area.
-
Patchy Hair Loss: The most distinctive sign of Tinea Capitis as it progresses is patchy hair loss. Affected areas of the scalp may begin to lose hair, creating bald spots. This is a result of the fungus invading the hair follicles, leading to hair breakage and weakening the hair shafts.
Patchy Hair Loss and Scalp Changes
One of the hallmark signs of Tinea Capitis is patchy hair loss. The infection damages the hair follicles, causing the hair to break off at the scalp level. This can result in uneven hair loss in the form of bald patches or small circular areas where the hair has fallen out.
-
Patches: These areas of hair loss may start as small, round patches, but they can increase in size as the infection spreads. The scalp in these areas might appear red, irritated, and scaly.
-
Scalp Texture: The texture of the scalp may also change in the affected areas, becoming rough or bumpy as the infection disrupts the hair follicles. These changes can lead to permanent scarring if left untreated.
Painful Swelling and Pus (Kerion)
In more severe cases, particularly with inflammatory Tinea Capitis, the infection can trigger a kerion, which is a severe inflammatory reaction. This is considered one of the most painful forms of Tinea Capitis.
-
Painful Swelling: The scalp becomes highly inflamed, and large, painful swelling may develop. This swelling can feel tender to the touch and can be quite uncomfortable, especially during daily activities like brushing the hair or wearing hats.
-
Pus-filled Abscesses: The inflammation caused by the kerion may lead to the formation of pus-filled abscesses or blisters on the scalp. These abscesses can rupture, releasing yellowish or greenish fluid and may have an unpleasant odor.
-
Increased Redness: The inflamed area of the scalp may become extremely red and swollen, and the skin may appear shiny due to the excessive fluid build-up.
Kerion is often associated with Trichophyton mentagrophytes and is more common in children, although it can occur in adults as well. Prompt medical attention is required to treat this severe form of Tinea Capitis, as it can lead to permanent hair loss and scarring.
Permanent Hair Loss and Scarring
If Tinea Capitis is left untreated or poorly managed, it can result in permanent hair loss and scarring. The fungus damages the hair follicles, leading to irreversible hair loss in the affected areas. The longer the infection remains untreated, the higher the chances that scarring will occur.
-
Scarring: The inflammation caused by the fungal infection can cause the scalp tissue to become scarred, making it difficult for hair to regrow. These scars may appear as shiny, smooth patches on the scalp where hair has been permanently lost.
-
Irreversible Bald Spots: Over time, the fungal infection may cause large, irregular bald patches that may not heal, even with treatment. These bald spots are often the result of long-standing inflammation or the damage caused by kerion.
Associated Symptoms (Lymph Node Swelling, Secondary Infections)
In some cases, secondary infections and other symptoms can accompany Tinea Capitis, especially if the infection is severe or left untreated.
-
Lymph Node Swelling: As the body fights the fungal infection, nearby lymph nodes may become swollen. This is a common response to infection and can occur in the neck or behind the ears. Swollen lymph nodes can be tender to the touch and may indicate that the body is attempting to combat the infection.
-
Secondary Bacterial Infections: When the scalp is scratched or irritated due to the constant itching, it can lead to secondary bacterial infections. Scratching can break the skin, allowing bacteria to enter, leading to additional redness, pus formation, and discomfort. These bacterial infections may require separate treatment with antibiotics.
-
Fever and Malaise: In rare cases, especially with severe infections like kerion, individuals may experience general symptoms like fever, fatigue, and malaise (general unwellness), which are signs that the infection has become systemic and may need urgent medical care.
Diagnosis
Diagnosing Tinea Capitis requires a combination of clinical evaluation, diagnostic tests, and differentiation from other scalp conditions. Due to the wide range of symptoms and the overlap with other scalp issues, accurate diagnosis is essential for selecting the most appropriate treatment. Below are the key diagnostic methods used to identify Tinea Capitis.
Clinical Evaluation (Physical Signs)
The first step in diagnosing Tinea Capitis is a thorough clinical evaluation by a healthcare professional. The doctor will assess the physical signs of the scalp and surrounding areas, such as:
-
Patchy Hair Loss: One of the most notable signs of Tinea Capitis is patchy hair loss. The doctor will look for areas of hair breakage or thinning, often accompanied by scaling, redness, and inflammation.
-
Itching and Redness: Itching on the scalp is a key symptom of the infection, and the doctor will examine the scalp for signs of irritation or redness, which are common in both non-inflammatory and inflammatory forms of Tinea Capitis.
-
Abscesses or Pustules: In more severe forms like kerion, the doctor will check for the presence of painful abscesses or pus-filled blisters. The presence of such lesions points to a more advanced or inflammatory stage of the infection.
During the clinical evaluation, the doctor will also inquire about potential exposure to infected individuals, pets, or environments where the infection may have been contracted. Understanding the patient’s history can significantly aid in the diagnosis.
Diagnostic Tests
To confirm the diagnosis of Tinea Capitis and rule out other conditions, several diagnostic tests may be performed. These tests help to identify the specific fungi responsible for the infection and determine the best course of treatment.
Wood’s Lamp Examination
A Wood's lamp examination is one of the simplest and most effective tools for diagnosing Tinea Capitis. This diagnostic tool uses ultraviolet (UV) light to illuminate the scalp. Some fungi, such as Microsporum canis, which is a common cause of Tinea Capitis, fluoresce under this light, producing a characteristic greenish glow.
-
Fluorescence: The presence of fluorescence is indicative of a fungal infection and can help distinguish it from other conditions. However, not all fungi will fluoresce under the Wood’s lamp, so this method is typically used in conjunction with other diagnostic tests.
Microscopy (KOH Preparation)
Microscopy is one of the most reliable methods for diagnosing Tinea Capitis. During this test, a sample of scalp scraping or hair is taken from the affected area. The sample is then treated with potassium hydroxide (KOH) to dissolve the skin and hair cells, making the fungal elements visible under a microscope.
-
Hyphae and Spores: Under the microscope, dermatophytes appear as hyphae (branching filaments) and spores. The presence of these fungal elements confirms the diagnosis of Tinea Capitis.
Microscopy is particularly useful for identifying Trichophyton and Microsporum, the two most common dermatophytes responsible for Tinea Capitis.
Fungal Culture
Fungal culture is a definitive diagnostic test used to isolate and identify the specific fungus causing the infection. A sample of scalp skin or hair is cultured in a laboratory to allow the fungal spores to grow. Once the fungus grows, it can be identified based on its morphological characteristics.
-
Identification: The fungal species can be identified, allowing the healthcare provider to determine the most effective antifungal treatment. While culture tests take longer to process (usually 1-3 weeks), they are extremely valuable for confirming the diagnosis and identifying any drug-resistant strains.
Fungal cultures are especially important in cases of persistent or recurrent Tinea Capitis, where other tests may not provide sufficient detail.
Molecular Tests (PCR)
Polymerase Chain Reaction (PCR) testing is a highly sensitive and specific method for diagnosing Tinea Capitis. This test detects the DNA of the fungus in the scalp scraping or hair sample. PCR is particularly useful for identifying fungal infections caused by species that are difficult to culture or identify using traditional methods.
-
Sensitivity: PCR is known for its high sensitivity and is capable of detecting low levels of fungal DNA, even when the infection is not visibly severe. This makes it an ideal diagnostic tool for cases where the infection is mild but still requires treatment.
PCR testing is not commonly used in routine clinical settings due to its cost and complexity but can be extremely helpful in specialized or persistent cases.
Trichoscopy (Dermoscopic Imaging)
Trichoscopy is a type of dermoscopic imaging used to examine the scalp and hair follicles in detail. Using a specialized dermoscope, the healthcare provider can examine the scalp at a microscopic level to identify subtle signs of fungal infections.
-
Fungal Signs: During a trichoscopy exam, the healthcare provider may observe yellowish crusts, scalp inflammation, or broken hair shafts indicative of Tinea Capitis. While not a diagnostic tool in itself, trichoscopy can provide additional information to support the diagnosis and help distinguish Tinea Capitis from other scalp conditions like seborrheic dermatitis or psoriasis.
Differential Diagnosis (Distinguishing from Other Scalp Conditions)
Because Tinea Capitis shares many symptoms with other scalp conditions, it is important to differentiate it from other possible diagnoses. Some common conditions that may resemble Tinea Capitis include:
-
Seborrheic Dermatitis: This condition causes itchy, scaly patches on the scalp and is often confused with Tinea Capitis. However, seborrheic dermatitis typically doesn’t involve hair loss or redness to the same extent as Tinea Capitis and does not respond to antifungal treatments.
-
Psoriasis: Psoriasis can cause scaly, red patches on the scalp, which can resemble the symptoms of Tinea Capitis. However, psoriasis tends to affect other areas of the body as well, and its scales are often thicker than those seen in Tinea Capitis.
-
Alopecia Areata: This condition causes smooth, round patches of hair loss, which may look similar to Tinea Capitis. However, alopecia areata is an autoimmune condition, not a fungal infection, and requires a different treatment approach.
-
Lupus: A skin condition like lupus can also cause scaly, hairless patches on the scalp, but it typically involves other systemic symptoms and is diagnosed through blood tests.
To avoid misdiagnosis, it is essential to use a combination of clinical evaluation and diagnostic tests to confirm the presence of Tinea Capitis and distinguish it from other conditions with similar symptoms.
Treatment Options
Tinea Capitis, or scalp ringworm, is a treatable condition, but it requires proper management to prevent complications such as permanent hair loss and scarring. The key to successful treatment is early intervention and consistent therapy. Below are the treatment options available for managing Tinea Capitis, ranging from oral medications to home care strategies.
Importance of Early and Complete Treatment
Early and complete treatment is crucial in preventing the infection from worsening and spreading. If left untreated, Tinea Capitis can lead to permanent hair loss, scarring, and even secondary bacterial infections. The infection is highly contagious, so timely treatment helps prevent transmission to others, especially in communal settings such as schools, daycare centers, or family environments.
It is important to complete the entire course of treatment, even if symptoms improve before the treatment ends. Incomplete treatment can lead to the infection returning, sometimes with increased resistance to antifungal medications.
Oral Antifungal Medications (Systemic Therapy)
Oral antifungal medications are the cornerstone of treatment for Tinea Capitis. These medications target the root cause of the infection—the dermatophytes—and are more effective than topical treatments for this type of fungal infection.
-
Griseofulvin: One of the most commonly prescribed oral antifungals for Tinea Capitis is griseofulvin. It works by disrupting the cell division of the fungi, preventing them from reproducing and spreading. It is typically prescribed for 6 to 8 weeks, depending on the severity of the infection.
-
Terbinafine: Terbinafine is another effective oral antifungal, known for its ability to inhibit fungal cell growth. It is often used as an alternative to griseofulvin and may be preferred in certain cases due to its shorter treatment duration.
-
Itraconazole and Fluconazole: These antifungals are sometimes used in resistant cases or in individuals who cannot tolerate other medications. They are effective against a broad range of dermatophytes and may be prescribed based on the patient’s specific needs.
Oral antifungals work from the inside out, clearing the infection more effectively than topical treatments alone. However, these medications can have side effects, including gastrointestinal upset, headaches, and liver toxicity in rare cases, so they should be used under medical supervision.
Topical Treatments (Adjunctive Role)
While oral antifungal medications are the primary treatment for Tinea Capitis, topical treatments can play an adjunctive role in managing the infection. These treatments are often used alongside oral medications to reduce symptoms and speed up recovery.
-
Antifungal Shampoos: Ketoconazole or selenium sulfide shampoos are commonly used to help reduce the fungal load on the scalp. These shampoos can be applied directly to the scalp and left on for several minutes before rinsing. They help to clear surface fungi and reduce the chances of spreading the infection to others.
-
Topical Antifungal Creams: In some cases, antifungal creams may be applied to small areas of the scalp that are not responding to oral treatment. While these are not as effective for Tinea Capitis as oral antifungals, they can help treat mild or localized cases of the infection.
-
Adjunctive Topical Treatments: When used in combination with oral medications, topical treatments can improve symptom management and help soothe scalp irritation, but they are not typically sufficient as standalone treatments for Tinea Capitis.
Duration of Therapy
The duration of therapy for Tinea Capitis depends on the severity of the infection and the specific treatment regimen used. Typically, oral antifungal therapy is required for 6 to 8 weeks to fully eradicate the infection. It is important to complete the entire course of medication to prevent the infection from returning or becoming resistant to the treatment.
For mild cases, if topical treatments are used in conjunction with oral therapy, the duration may be shorter. However, for severe infections, especially those with kerion or secondary bacterial infections, treatment duration may be extended and will require close monitoring.
Managing Severe Cases (Kerion, Steroid Use)
In cases of kerion, which is a severe, inflammatory reaction that leads to pus-filled abscesses and extreme swelling, immediate intervention is required. Kerion can result in permanent hair loss and scarring if not treated aggressively.
-
Steroids: In some severe cases, systemic steroids may be prescribed to reduce inflammation and swelling. Steroids help in controlling the immune response, preventing further tissue damage. However, steroids are typically used for short durations and only when absolutely necessary, as they can suppress the body's ability to fight the infection.
-
Antibiotics for Secondary Infection: Since kerion may also lead to secondary bacterial infections, antibiotics are often prescribed to manage these infections. This combination of antifungal and antibacterial treatment is essential to prevent complications.
-
Close Monitoring: Severe cases of Tinea Capitis, especially kerion, require close monitoring by a healthcare professional to ensure the infection is properly managed and to prevent permanent damage.
Monitoring and Follow-Up
Regular follow-up appointments are critical to ensure that treatment is effective and to check for any potential complications, such as secondary bacterial infections or hair loss due to scarring. Your healthcare provider may recommend additional scalp scrapings or microscopic examinations to ensure the infection has been completely cleared.
-
Success Indicators: After a few weeks of treatment, a reduction in itching, redness, and scaling should be observed. Hair regrowth should begin within a few months, although it can take up to 6 months for the scalp to fully recover in severe cases.
-
Treatment Adjustments: If the infection does not improve with the prescribed treatment, your healthcare provider may adjust your medication regimen or conduct further tests to identify any resistant fungal strains.
Home Care and Hygiene Measures
While medical treatment is essential, good home care and hygiene practices can help prevent the spread of Tinea Capitis and improve treatment outcomes. Key hygiene measures include:
-
Avoid Sharing Personal Items: To prevent the infection from spreading, avoid sharing combs, towels, hats, or any other personal items that may come into contact with the infected area.
-
Regular Scalp Washing: Wash the scalp regularly with antifungal shampoos as recommended by your healthcare provider. This will help reduce the fungal load and prevent reinfection.
-
Clean Bedding and Personal Items: Wash bedding, pillows, and clothing regularly to eliminate any potential fungal spores that may be present. It's essential to disinfect these items to prevent reinfection.
-
Maintain a Clean Environment: Keeping the home environment clean, particularly in shared spaces, helps prevent the transmission of the infection to family members or other individuals.
By combining medical treatment with hygiene practices, individuals with Tinea Capitis can effectively manage the infection and reduce the risk of recurrence.
Prevention and Control
Preventing Tinea Capitis, commonly known as scalp ringworm, involves a combination of personal hygiene practices, environmental cleanliness, and awareness of potential sources of infection. Given its highly contagious nature, especially among children, implementing preventive measures is crucial to reduce the spread of this fungal infection.
How to Prevent Tinea Capitis
-
Maintain Regular Scalp Hygiene: Washing the hair regularly with antifungal shampoos containing ingredients like selenium sulfide or ketoconazole can help reduce fungal spores on the scalp. These shampoos are particularly beneficial for individuals at higher risk or those living in areas with prevalent fungal infections.
-
Practice Proper Hand Hygiene: Frequent handwashing with soap and water, especially after touching potentially contaminated surfaces or animals, can significantly reduce the risk of transferring fungal spores to the scalp.
-
Educate on Personal Hygiene: Teaching children and adults the importance of personal hygiene, including not sharing personal items and maintaining clean hair and scalp, is essential in preventing Tinea Capitis.
Personal Hygiene and Hair Care
-
Avoid Sharing Personal Items: Items such as combs, brushes, hats, towels, and pillows should not be shared, as they can harbor fungal spores and facilitate the spread of the infection.
-
Clean Hair Accessories Regularly: Disinfect combs and brushes by soaking them in a mixture of bleach and water (1:10 ratio) for at least 1 hour daily during the first few days of treatment.
-
Wash Bedding and Towels Frequently: Launder all bedding, towels, and clothing in hot water with soap to eliminate any fungal spores.
Avoiding Sharing Personal Items
-
Do Not Share Personal Care Items: Avoid sharing items like hairbrushes, combs, hats, and towels, as these can transfer fungal spores from one person to another.
- Use Personal Items Exclusively: Ensure that each individual uses their own personal items and does not lend them to others, particularly in communal settings.
Cleaning and Disinfecting Household Items
-
Disinfect Contaminated Items: Items that may have come into contact with an infected individual, such as combs, brushes, and bedding, should be thoroughly cleaned and disinfected.
-
Use Effective Disinfectants: Household bleach diluted appropriately can be used to disinfect surfaces and items. Ensure that the disinfectant is effective against dermatophytes and follow the manufacturer's instructions.
Managing Pets and Animal Contact
-
Regular Veterinary Check-ups: Pets, especially cats and dogs, should be regularly checked by a veterinarian for signs of ringworm, as they can be carriers of the fungus.
-
Limit Contact with Infected Animals: Avoid close contact with pets that show signs of skin infections until they have been treated and cleared by a veterinarian.
-
Disinfect Pet-Related Items: Regularly clean and disinfect pet bedding, grooming tools, and areas where pets frequent to prevent the spread of fungal spores.
School and Community Measures
-
Inform Educational Institutions: If a child is diagnosed with Tinea Capitis, inform the school so that appropriate measures can be taken to prevent the spread among other children.
-
Avoid Sharing Sports Equipment: In community settings like sports teams, ensure that equipment such as helmets and pads are not shared unless they have been properly disinfected.
-
Promote Awareness and Education: Educate community members about the signs, symptoms, and preventive measures of Tinea Capitis to encourage early detection and treatment.
Implementing these preventive measures can significantly reduce the risk of contracting or spreading Tinea Capitis. Regular hygiene practices, proper cleaning protocols, and awareness are key components in controlling this fungal infection.
Complications of Tinea Capitis
Tinea Capitis, commonly known as scalp ringworm, is a fungal infection that primarily affects the scalp and hair follicles. While it is treatable, if left unmanaged or inadequately treated, it can lead to several complications that impact both physical and emotional well-being.
Scarring and Permanent Hair Loss
One of the most concerning complications of Tinea Capitis is scarring alopecia, which results from inflammation and damage to the hair follicles. Inflammatory forms of the infection, such as kerion and favus, can cause severe tissue damage, leading to permanent hair loss in the affected areas. This scarring is irreversible, meaning that hair will not regrow in these regions. Even after successful treatment, the aesthetic impact of bald patches can be long-lasting.
Secondary Bacterial Infections
The inflamed and broken skin caused by Tinea Capitis provides an entry point for bacteria, leading to secondary infections. These bacterial infections can exacerbate the condition, causing increased redness, swelling, pus formation, and pain. In severe cases, untreated bacterial infections may lead to systemic complications, requiring more intensive treatment.
Psychological Impact
Beyond the physical symptoms, Tinea Capitis can have significant psychological effects. Individuals, especially children, may experience reduced self-esteem and social anxiety due to visible hair loss and scalp lesions. The stigma associated with visible scalp conditions can lead to social withdrawal, bullying, and emotional distress. Long-term psychological impacts have been observed, particularly in cases where hair loss is severe or persistent.
Chronic or Recurrent Infections
In some instances, Tinea Capitis can become chronic or recurrent. This may occur due to inadequate treatment, non-compliance with prescribed therapies, or reinfection from untreated household members or pets. Chronic infections can lead to prolonged symptoms and an increased risk of complications, including scarring and psychological distress.
Tinea Capitis in Special Populations
Tinea Capitis, commonly known as scalp ringworm, predominantly affects children but can also occur in adults, especially in certain high-risk groups. Understanding how this fungal infection manifests and is managed in these populations is crucial for effective prevention and treatment.
Adults (Especially Postmenopausal Women)
While Tinea Capitis is rare in adults, postmenopausal women are notably more susceptible. This increased risk is attributed to hormonal changes that alter scalp sebum composition, reducing its protective properties and making the scalp more vulnerable to fungal infections. Additionally, postmenopausal women often experience thinning hair, which can facilitate fungal invasion. The infection in adults may present atypically, resembling conditions like seborrheic dermatitis, folliculitis, or lupus erythematosus, leading to potential misdiagnosis and delayed treatment.
Immunocompromised Individuals
Individuals with weakened immune systems, such as those with HIV/AIDS, diabetes, systemic lupus erythematosus, or those undergoing immunosuppressive therapy, are at a heightened risk for Tinea Capitis. In these individuals, the infection may be more severe, persistent, and resistant to standard treatments. The clinical presentation can vary, and the condition may not respond to typical antifungal therapies, necessitating specialized medical attention.
Outbreaks in Schools, Daycares, and Households
Tinea Capitis is highly contagious and can spread rapidly in communal settings like schools, daycare centers, and households. Outbreaks often occur when infected individuals share personal items such as combs, hats, or towels, or have close physical contact. In such environments, it's essential to implement strict hygiene practices, including regular handwashing, avoiding the sharing of personal items, and ensuring that affected individuals receive appropriate treatment to prevent further transmission.
Myths and Facts about Tinea Capitis
Tinea Capitis, commonly known as scalp ringworm, is a fungal infection that affects the scalp and hair follicles. Despite its prevalence, several misconceptions surround this condition. Understanding the facts can help in early detection, effective treatment, and prevention.
Common Myths about Tinea Capitis
-
Myth: Tinea Capitis is caused by worms.
-
Fact: Despite its name, Tinea Capitis is not caused by worms. It is a fungal infection caused by dermatophytes, primarily Trichophyton and Microsporum species.
-
-
Myth: Only children get Tinea Capitis.
-
Fact: While Tinea Capitis is more common in children, adults can also be affected, especially those with compromised immune systems or close contact with infected individuals.
-
-
Myth: Tinea Capitis isn't contagious.
-
Fact: Tinea Capitis is highly contagious and can spread through direct contact with an infected person or animal, or by sharing personal items like combs, hats, or towels.
-
-
Myth: Once you've had Tinea Capitis, you're immune.
-
Fact: Having had Tinea Capitis does not provide immunity. Reinfection is possible if exposed to the fungus again.
-
-
Myth: Tinea Capitis is always easy to diagnose.
-
Fact: Tinea Capitis can be challenging to diagnose, especially in adults, as it may mimic other scalp conditions like seborrheic dermatitis or psoriasis.
-
-
Myth: Applying hair oil before a fungal culture affects test results.
-
Fact: Recent studies have shown that using hair oil does not significantly affect the sensitivity of fungal cultures in detecting Trichophyton tonsurans in pediatric patients.
-
-
Myth: Tinea Capitis can be treated effectively with over-the-counter shampoos alone.
-
Fact: While medicated shampoos can help reduce fungal load, oral antifungal medications are typically required for effective treatment of Tinea Capitis.
-
-
Myth: Tinea Capitis is a rare condition.
-
Fact: Tinea Capitis is a common fungal infection, particularly among children, and can lead to complications if not treated promptly.
-
-
Myth: Tinea Capitis always causes visible hair loss.
-
Fact: Not all cases of Tinea Capitis result in visible hair loss. Some individuals may experience only mild symptoms like itching or scaling without noticeable hair thinning.
-
-
Myth: Tinea Capitis is not a serious condition.
-
Fact: If left untreated, Tinea Capitis can lead to complications such as permanent hair loss, scarring, and secondary bacterial infections.
-
Conclusion
Tinea Capitis, commonly known as scalp ringworm, is a prevalent fungal infection affecting individuals of all ages, particularly children. Recognizing its causes, symptoms, and treatment options is crucial for effective management and prevention.
Causes and Pathogenesis
The infection is primarily caused by dermatophytes, with Trichophyton and Microsporum species being the most common culprits. These fungi invade the hair follicles and surrounding skin, leading to inflammation and hair loss. Transmission occurs through direct contact with infected individuals or contaminated objects.
Symptoms
Common signs include itchy, scaly patches on the scalp, hair loss, and redness. In severe cases, painful, pus-filled swellings known as kerion may develop, leading to scarring and permanent hair loss.
Diagnosis
Diagnosis is based on clinical examination and confirmed through tests such as Wood's lamp examination, KOH preparation, fungal culture, and PCR analysis. Trichoscopy, or dermoscopic imaging, can also aid in identifying characteristic features of the infection.
Treatment
The primary treatment involves oral antifungal medications, typically administered for 4 to 6 weeks. Topical treatments may be used adjunctively. In severe cases, corticosteroids may be prescribed to reduce inflammation. Adherence to the full course of treatment is essential to prevent recurrence.
Prevention
Preventive measures include maintaining good personal hygiene, avoiding sharing personal items like combs and hats, and cleaning and disinfecting household items. Managing pets and animal contact is also important, as animals can harbor the fungi. In communal settings such as schools and daycares, prompt identification and treatment of infected individuals can help control outbreaks.
By understanding Tinea Capitis and implementing appropriate preventive and treatment strategies, individuals can effectively manage and reduce the spread of this fungal infection.
Frequently Asked Questions
What is Tinea Capitis?
Tinea Capitis, commonly known as scalp ringworm, is a fungal infection affecting the scalp and hair follicles. It's caused by dermatophytes, primarily Trichophyton and Microsporum species. Despite its name, it's not caused by a worm. The infection leads to symptoms like itchy, scaly patches, hair loss, and redness on the scalp. It's highly contagious, especially among children aged 3 to 14, and can spread through direct contact or shared personal items.
How does Tinea Capitis spread?
Tinea Capitis spreads through direct contact with an infected person or animal, or by sharing contaminated items like combs, hats, or towels. The fungi can live on surfaces and hair for extended periods, making it easy to transmit in communal settings such as schools or daycare centers.
What are the symptoms of Tinea Capitis?
Symptoms include itchy, scaly patches on the scalp, hair loss, redness, and sometimes swollen lymph nodes. In severe cases, pus-filled swellings known as kerion may develop, leading to scarring and permanent hair loss.
How is Tinea Capitis diagnosed?
Diagnosis involves a physical examination of the scalp, Wood's lamp examination, KOH preparation, fungal culture, and PCR analysis. Trichoscopy, or dermoscopic imaging, can also aid in identifying characteristic features of the infection.
What are the treatment options for Tinea Capitis?
Treatment typically includes oral antifungal medications like griseofulvin, terbinafine, or itraconazole, usually administered for 4 to 6 weeks. Topical treatments may be used adjunctively. In severe cases, corticosteroids may be prescribed to reduce inflammation.
Can Tinea Capitis be prevented?
Preventive measures include maintaining good personal hygiene, avoiding sharing personal items like combs and hats, cleaning and disinfecting household items, and managing pets and animal contact. In communal settings such as schools and daycares, prompt identification and treatment of infected individuals can help control outbreaks.
Is Tinea Capitis common in adults?
While Tinea Capitis is more common in children, adults can also be affected, especially those with compromised immune systems or close contact with infected individuals. In adults, the infection may present atypically, resembling conditions like seborrheic dermatitis or folliculitis.
What are the complications of Tinea Capitis?
Complications can include scarring and permanent hair loss, secondary bacterial infections, psychological impact such as reduced self-esteem, and chronic or recurrent infections. Prompt treatment is essential to prevent these complications.
How long does it take to recover from Tinea Capitis?
With appropriate treatment, most individuals begin to see improvement within 2 to 4 weeks. However, complete resolution may take several weeks to months. It's crucial to complete the full course of treatment to ensure the infection is fully eradicated.
10. Can Tinea Capitis recur?
Yes, Tinea Capitis can recur, especially if the initial infection wasn't completely treated, if reinfection occurs from untreated household members or pets, or if preventive measures aren't followed. Recurrent infections may require a longer or different treatment regimen.
Is Tinea Capitis contagious?
Yes, Tinea Capitis is highly contagious and can spread through direct contact with an infected person or animal, or by sharing contaminated items like combs, hats, or towels. Good hygiene practices and avoiding sharing personal items can help prevent transmission.
Can Tinea Capitis affect pets?
Yes, pets, especially cats and dogs, can harbor the fungi that cause Tinea Capitis. It's important to have pets checked for ringworm and treated if necessary to prevent transmission to humans.
What should I do if my child has Tinea Capitis?
If your child has Tinea Capitis, consult a healthcare provider for diagnosis and appropriate treatment. Ensure your child completes the full course of prescribed medication, maintain good hygiene practices, and prevent sharing personal items to reduce the risk of spreading the infection.
Can Tinea Capitis be mistaken for other conditions?
Yes, Tinea Capitis can be mistaken for other scalp conditions like seborrheic dermatitis, psoriasis, or folliculitis due to similar symptoms. A thorough examination and appropriate diagnostic tests are essential for accurate diagnosis.
When should I see a doctor for Tinea Capitis?
You should see a doctor if you or your child develop symptoms of Tinea Capitis, such as itchy, scaly patches on the scalp, hair loss, or redness. Early diagnosis and treatment are crucial to prevent complications and reduce the risk of spreading the infection.





