Fungal Acne : Symptoms, Causes, Treatment & Prevention

Table of Contents
-
Fungal acne: An overview
-
What are the Symptoms of Fungal Acne?
-
What are the Causes of Fungal Acne?
-
How to Treat Fungal Acne?
-
Prevention from Fungal Acne
-
When to consult a doctor?
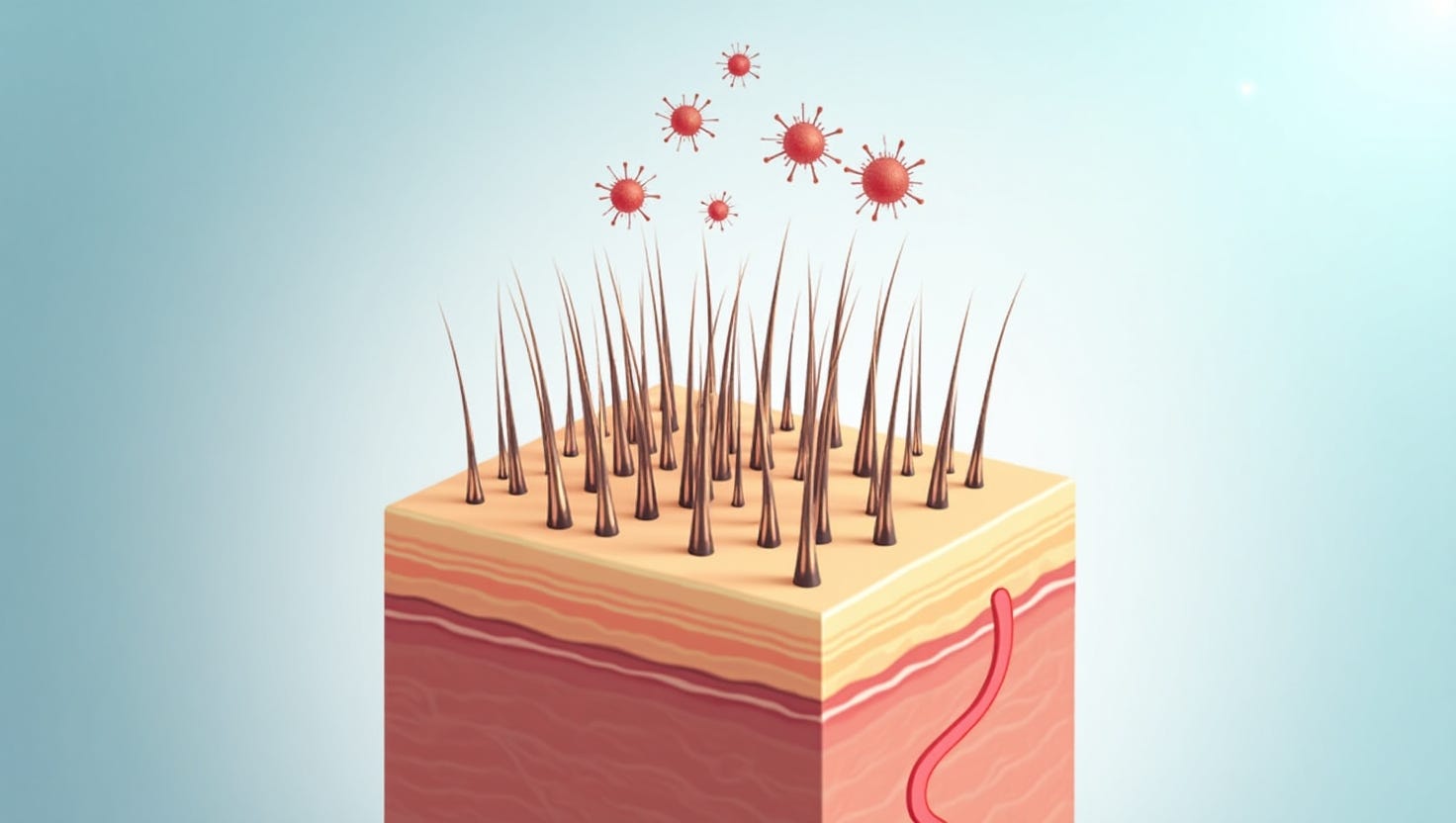
Fungal Acne: An Overview
The hair follicles on your skin might become infected with a fungus, causing fungal acne. The most frequent symptom is itching, paired with little, uniformly shaped pimples. Whiteheads and skin irritation can result from fungus-induced acne. Acne vulgaris and it are frequently mistaken. Most often, blackheads and whiteheads are present with this form of acne.
Fungal acne may affect anyone. Young adults frequently have oily skin where yeast thrives and are the most likely to experience it. The yeast multiplies swiftly on warm, wet, or perspirant skin.
What Are The Symptoms Of Fungal Acne?
Small pimples pop out suddenly due to fungal acne, giving the appearance of a rash. The lumps seem clustered and are similar in size and shape. There may be a red ring or border surrounding each pimple.
Your skin might feel like -
-
Burning.
-
Itchy.
-
Painful
Although the blemishes can appear anywhere on your skin, they are most frequently found on the
-
Chin.
-
Chest.
-
Forehead.
-
Neck.
-
Upper arms.
-
Shoulders.
-
Back region.
What Are The Causes Of Fungal Acne?
Acne caused by fungus is a bit of a misnomer. Contrary to acne, fungal acne is not primarily brought on by oil and bacteria in pores. However, the creation of oil and sebum plays a significant role in supplying the bacteria that cause fungal acne with food.
Instead, a fungus called yeast overgrowth is to be blamed for the pimple-like lumps and inflamed skin associated with fungal acne.
Malassezia yeast is naturally present on almost everyone's skin. But when yeast enters damaged or obstructed hair follicles, the fungus can become a problem.
Follicles may suffer damage because of:
-
Having excessive skin-to-skin contact.
-
Leaving skin warm and wet.
-
Using wax, razors, or other hair removal methods.
-
Constant skin contact or skin rubbing.
-
Using a spa or whirlpool.
-
Wearing tight clothing.
Antibiotic usage can either result in the development of fungal acne or exacerbate it. On the skin, both bacteria and yeast exist. Antibiotics, however, can reduce the population of beneficial bacteria and result in yeast overgrowth, which may result in fungal acne.
Your body has a more challenging time controlling yeast development if you have an immune system suppressed by illness or medication. These elements increase the likelihood of developing fungal acne.
How To Treat Fungal Acne?
When misdiagnosed as acne, fungus acne can persist for long.
With antifungal tablets or a lotion, a yeast infection can be treated most effectively. Your dermatologist can identify the issue since antibiotics are ineffective in treating this condition. They may also swab your skin to confirm the yeast infection. For addressing related skin concerns or scars left by previous skin conditions, professional Pimple Scar Treatment can help restore smoother, healthier skin with tailored solutions.
Other hygiene, self-care routines, and good-quality products that might benefit your skin may also be recommended by your dermatologist. You could
- Immediately change out of your sweaty workout attire.
- Right after your workout, take a shower.
- Wear loose-fitting garments made of natural materials like cotton, silk, or bamboo.
- Use your prescription as directed to promote hair growth.
Specific natural therapies can help clean up the blemishes and reduce the symptoms of fungal acne, including
-
Applying warm compresses to the affected region many times daily.
-
Putting an end to whatever is harming your hair follicles for approximately a month (for instance, take a vacation from shaving or do not wear tight clothing).
-
Before attempting any home cures, consult a doctor.
Prevention From Fungal Acne
The likelihood of developing fungal acne can be reduced by:
-
After working out, showering, and changing into new clothing.
-
When waxing, plucking, or shaving, be careful.
-
Use only pristine and well-maintained hot tubs.
-
between uses, you should wash and dry your bathing suit.
-
Wear loose clothing, particularly in hot and humid weather or when working out.
-
Your doctor could suggest using antifungal drugs over the long term if you experience recurrent fungal acne outbreaks.
Get in touch with a Kaya dermatologist if your suspected fungal acne outbreak hasn't cleared up after three weeks of home treatment.
Kaya's dermatologists offer specialized expertise to combat fungal acne effectively. Personalized treatments and carefully curated products from Kaya target the root causes of the condition, relieving the discomfort and unsightly appearance associated with fungal acne. For those dealing with lingering marks or scars left behind, professional Acne Scar Treatment ensures smoother and healthier skin. Trust our dermatological prowess to help you achieve clear, radiant skin. Say goodbye to fungal acne and hello to confidence and comfort with Kaya's expert care.